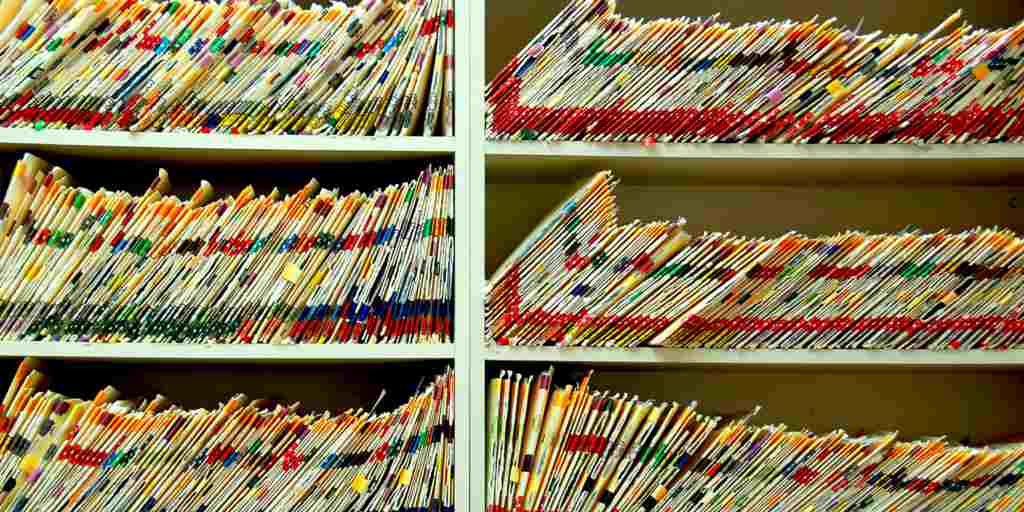
Years ago you could find patient charts on the oncology or transplant service that were a foot thick or more. Clerks placed everything coming in on a patient in the chart. This included various pending and interim reports, which usually duplicated content of cumulative reports. It only takes a few days for a large amount of clinical documentation to accumulate. There was so much congestion that the chart became essentially useless.
So why did this happen? Clerks found it very easy to put things in a chart but very difficult to remove anything. For some it was the belief that they might be punished if they acted on their own. They often did not have the time or understanding to make decisions as to what was useful or not. Often there were problems with supervision. It was just easier to go with the flow.
Promise of Electronic Health Record Systems
The electronic health record (EHR) was supposed to eliminate problems like this. The stacks of paper may be gone, but the clutter is still there. Just look at the record of anyone with multiple serious problems who has been in the hospital for a few days and try to find something. It is often harder than you might think unless the EHR is well-designed..
Patients with significant problems tend to accumulate diagnoses, and if no one is in charge then multiple entries are made for essentially the same problem, resulting in very long lists. Multiple providers will prescribe for the patient but will not want to stop anything started by someone else when they do not know why it was started. And pages of nursing notes can be added with the push of a button. Everything can be documented and usually is.
Fundamental Problems with Electronic Health Records
Many of the fundamental problems that plaqued paper charts persist. A patient may have too many providers, too many problems, too many medications. There is too much litigation, too little time, too little understanding and too little communication. Now, providers face different challenges: They have difficulty matching patients and records, there are no universal standards, and navigating the information in the EHR is a challenging too. There are warning boxes, and barriers to freely moving through the various screens of the EHR which sometimes makes it even more difficult to track down the essential information that is needed. Attitudes toward adoption are often more negative after use than they are pre-implementation, resulting in frustration, inefficiency and time waste. So what can be done?
Automated algorithms can help to solve some of these problems. Many studies have been carried out which explore the ways medical algorithms integrated into the EHR can improve efficiency and transform the EHR into an automatic tool for support. Algorithms can provide a knowledge-based classification system to manage and process data. For example, if each problem is ICD-10 encoded then it is straightforward to identify overlapping terms and to even suggest a replacement. Duplicate drug orders and drugs that do not have an indication documented can prompt mess ages to the prescriber for clarifiicaton, making deprescribing less difficult. People may have problems with information overload, but algorithms can handle the load just fine. Electronic health record optimization can be achieved through more efficient record keeping and documentation methods.
[button link=”http://www.medicalalgorithms.com/home/index?signup=1 ” color=”custom” size=”large” type=”” shape=”” target=”_self” title=”” gradient_colors=”#fb0303|” gradient_hover_colors=”#f47575|” accent_color=”” accent_hover_color=”” bevel_color=”” border_width=”1px” shadow=”” icon=”” icon_position=”left” icon_divider=”no” modal=”” animation_type=”0″ animation_direction=”left” animation_speed=”1″ alignment=”center” class=”” id=””]Free Account Sign Up[/button]