In September, 2015, the Institute of Medicine (IOM) released a report titled Improving Diagnosis in Health Care. This report is a follow up to earlier revealing reports published To Err is Human: Building a Safer Health System (2000) and Crossing the Quality Chasm: A New Health System for the 21st Century, (2001), which indicated that an unacceptable number of errors occurred in healthcare delivery. The current study outlines ways to improve diagnosis in healthcare.
Diagnostic Error Defined as Not Being Perfect
Any discussion has to start with a definition. The one chosen by the IOM committee has its share of nuances. First, a diagnostic error is defined as:
“….a failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patient.”
Basically an error is any deviation from the ideal, not just getting something wrong. With such a definition then it is easy to make the statement that most people will experience an “error” in their lifetime. Any baseball player who does not hit a home run every time at the plate must be a failure.
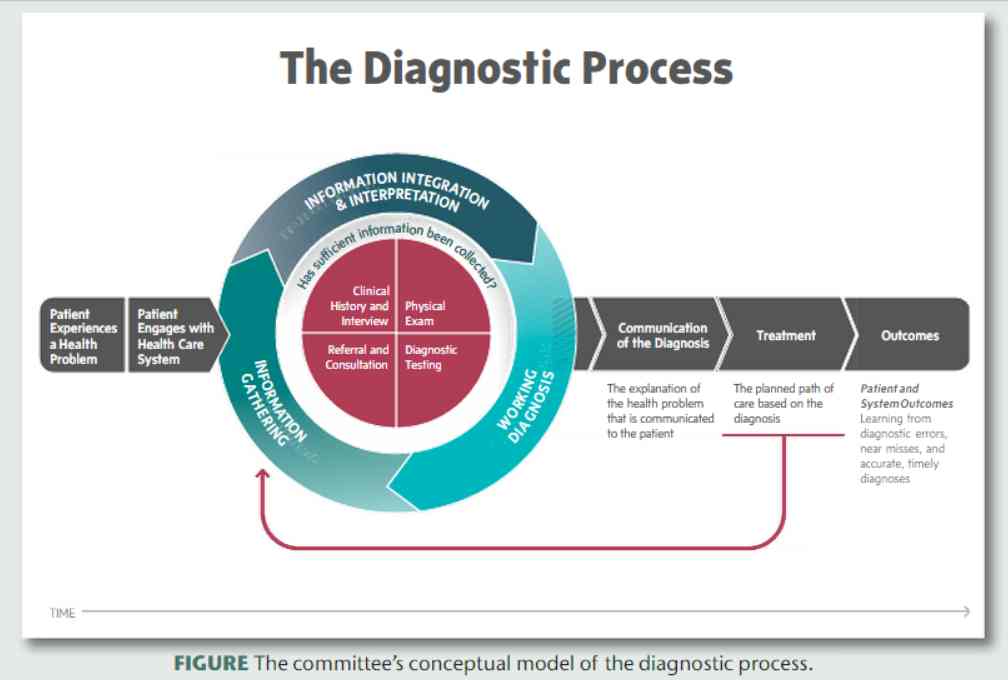
IOM has developed the Figure below to define the diagnostic process, which is linear once the diagnosis has been made.
This makes treatment and outcomes seem like mere afterthoughts, rather than integral to the diagnostic process. Many times a failure to achieve the expected goal is the only clue of a wrong or missing diagnosis. And the presence of unintended consequences from therapy is the basis for additional diagnoses.
Finally, the patient is a victim and not held accountable in any way. To be engaged as a member of the diagnostic team perhaps, but not someone to be held responsible for their behaviors.
Recommendations for Improving Diagnosis
The report makes certain recommendations for improving diagnosis. These can be divided into 3 groups – the achievable, the idealistic, and the academic.
Achievable goals include:
- Facilitating teamwork
- Enhancing education and training in the diagnosis process
- Making sure that health information technologies support diagnosis
- Identifying and learning from diagnostic errors and near misses
While achievable, the following goals seem more wishful:
- Creating a system and culture supportive of the diagnostic process
- Having a liability system that allows people to admit errors
Finally, no good academic is going to pass an opportunity to get a grant:
- Promote research to devise a better payment model
- Provide dedicated funding for research
Role for Automated Medical Algorithms and Other Technologies
Humans can only do so much because of inherent limitations. The only way to make real improvements (and to do it cost-effectively) is through technology.
Automated medical algorithms have a role in reaching the achievable goals. They can operate in the background, decreasing cognitive loads that may contribute to judgment errors. They can provide a readily available second opinion on diagnoses and can serve to document decisions in the medical record. They can be used for education and training. Since they are modular they can be easily replaced or repaired if found wanting.
To use medical algorithms effectively one needs a central data record, and the current system is fragmented. A central data record will solve many ills, but whether all patients will welcome such a system remains to be seen.
The other technologies that are needed are improved communication and tracking systems. It can be difficult to get a key diagnosis to everyone who needs to know. There is a need for secure reporting and better hand-off procedures, not to mention that the new and improved diagnosis is acted upon.
By incorporating automated medical algorithms and other communication technologies into the process, a reduction in diagnostic errors is possible and will result in better outcomes for all patients and healthcare providers.