Prior Authorization – Using Medical Algorithms to Increase Likelihood for Coverage
Evidence-based medical algorithms can help to streamline processes in physicians’ offices by speeding up the time it takes to get insurance prior authorizations from payers. Physicians can rely on medical algorithms to substantiate their decision-making, since each algorithm is backed by scientific, peer-reviewed, published evidence. Two cases below demonstrate how algorithms available online have helped to reduce paperwork and physician/staff time devoted to completing prior authorization forms.
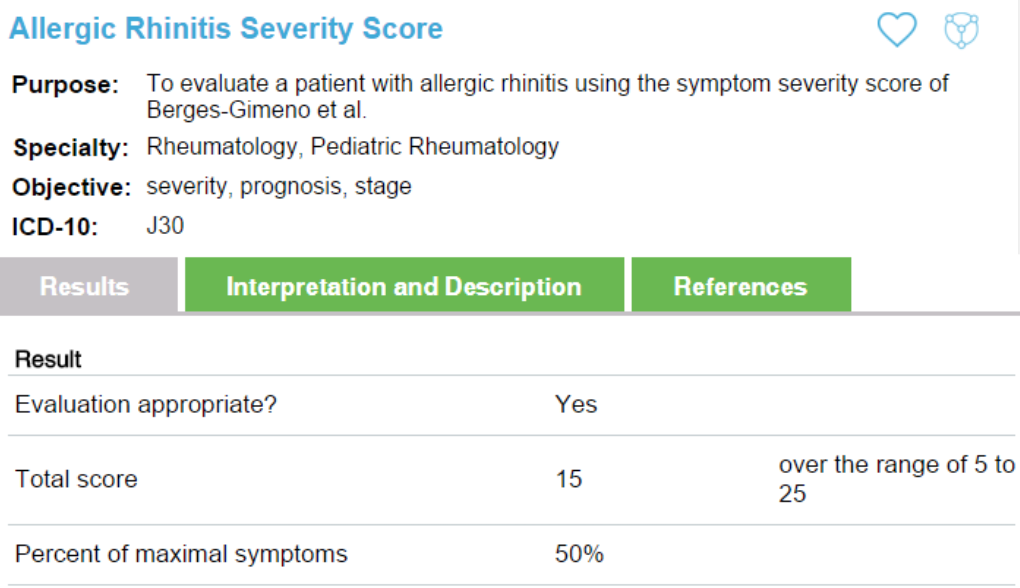
Case One: Allergic Rhinitis
A 12-year-old male with significant allergic rhinitis was seen for a follow-up visit. His current treatment of nasal steroid and oral antihistamine was not improving his symptoms and his quality of life was decreasing as a result of the symptoms. Montelukast had been trialed previously but was unable to be tolerated by the patient. Using the allergic rhinitis severity score algorithm, the symptom severity score was generated in a few seconds. The results, title of algorithm, purpose, objective, and ICD-10 code were all included in the online listing.
This information was attached to the patient’s insurance prior authorization form and the new combination nasal spray medication was approved without delay.
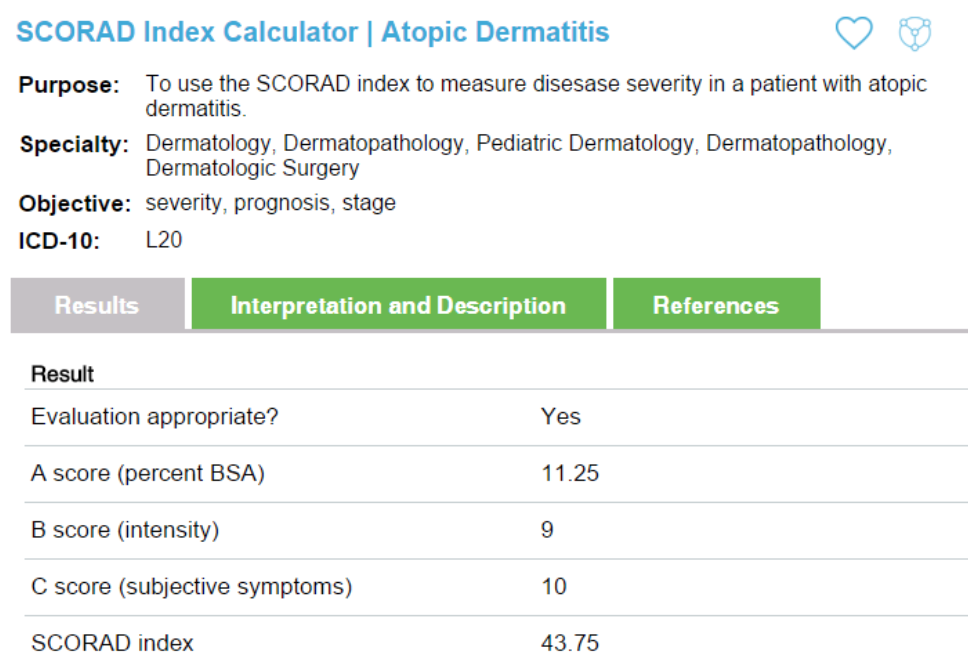
Case Two: Atopic Dermatitis
A 20-year-old female with atopic dermatitis, present since early in childhood, has been having worsening flare ups in the past 6 months. Despite trials with numerous over-the-counter and prescription topical emollients and topical steroids, her symptoms were still persistent. The itching was affecting her daily life and disturbing her sleep on occasion. Her physician decided to prescribe Pimecrolimus but her insurance company was refusing to cover the treatment. Initial discussions between the physician and the health insurance prior authorization department were not helpful. The decision was appealed and using the SCORAD Index Calculator available through The Medical Algorithms Company, the score, description of the result, and evidence-based article on which it is based was sent with the appeal form. This information was the deciding factor in having the prescription covered for this woman. She was extremely grateful for the assistance.
Nearly every primary care physician and staff member can attest to the difficulties dealing with insurance companies when it comes to prior authorizations or appeals for prescription medications or imaging. In our experience, using the clinical decision support algorithms available through The Medical Algorithms Company (www.MediclaAlgorithms.com) have reduced the number of denials, saved countless hours for myself and my staff, and improved the care for our patients.